-->
Incidence
1 in 2000 - 5000 live births (unknown Malaysian figures)
Bochdalek hernia most common, left sided (80%)
Morgagni hernia (2%) usually in older children
Embryology
-
Diaphragm fusion involves 4 layers:
o
Septum transversum anteriorly
o
Pleuroperitoneal membrane dorsolaterally
o
Esophageal mesentry
o
Muscular portion from intercostal muscles
-
Starts at 4th week of gestation
-
Completes at 8th week of gestation
-
Lungs develope as a derivative from foregut and forms a diverticulum. Two lung buds form at around 4th week of gestation.
- Airway differentiation developes up to 24 weeks of gestation. This is followed by appearance of pneumocyte I and II, the later responsible for secreting surfactant.
- Vascular deveopement occur concurrently with lung growth.
Pathology:
-
Gut herniates through the yolk sac and returns
into the abdominal cavity at 8 – 9th week of gestation.
-
Failure of closire of diaphragm results in
hernia
-
May cause obstruction to the esophagus
(resulting in polyhydroamnios)
-
Circulation maintained as fetus is dependant on
utero-placental-fetal circulation
-
After birth, adult type of circulation unable to
be achieved due to persistent raised pulmonary pressure and reduction in
pulmonary blood flow.
-
This results in right to left shunt resulting in
deoxygenated blood circulating in the system and results in increase in
pulmonary pressure.
Diagnosis
Antenatal:
Ultrasound
-
Stomach or other abdominal organ in the fetal
thorax
-
Polyhydromnios (80%)
At birth:
-
Respiratory distress
-
Scaphoid abdomen (need high index of suspicion)
-
Asymmetrical distended chest wall
-
Shifted heart sounds (‘Dextrocardia’ is CDH
until proven otherwise)
-
Absent breath sounds
-
Hypotension and peripheral hypoperfusion
(reduced venous return from caval compression)
-
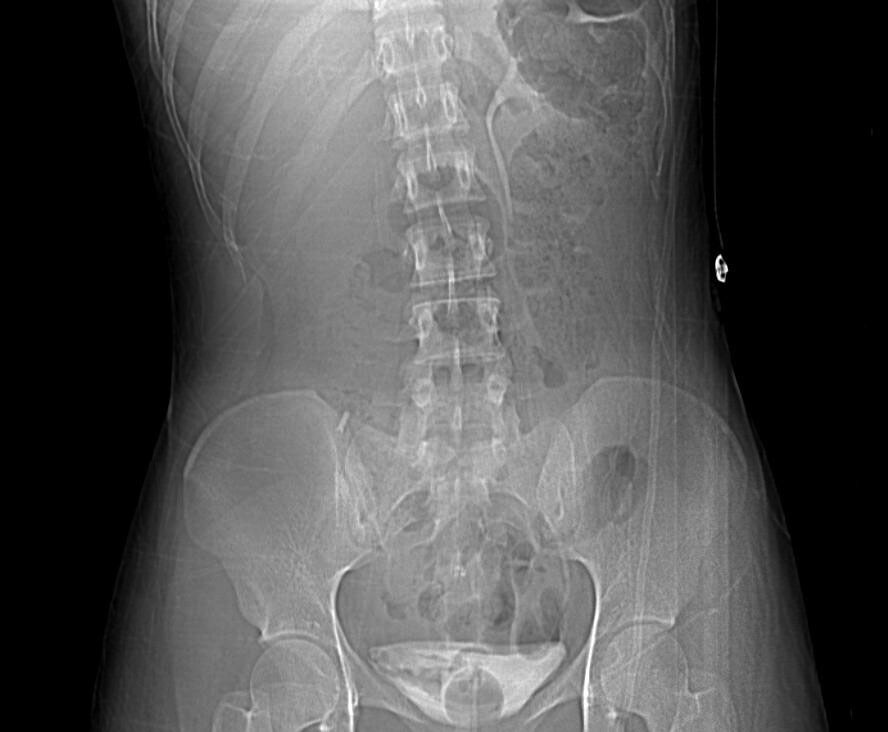
Chest X-ray: Loops of intestine or stomach in
chest wall. Clearer if NG tube inserted.
-
Contrast studies might be indicated in certain
cases but usually not necessary.
Some late presentations present with chronic lung disease,
recurrent coughs, pneumonia.
 |
| Notice the heart on the right side and the nasogastric tube tip ending in the thorax. |
Associated Anomalies
High incidence of lethal congenital anomalies asociated with
CDH
-
Skeletal defects (32%)
-
Cardiac anomalies (24%)
-
Tracheobronchial anomalies (18%)
-
Neural tube defects
Differential Diagnosis:
Eventration of the diaphragm (weakness of the diaphragm ie. Phrenic
nerve injury)
Management
Antenatal:
-
Tertiary center delivery with well equiped NICU
and pediatric surgery support.
-
Transport to be made in-utero.
-
Parent counselling
-
Amnicentesis for karyotyping if suspected
congenital anomaly
-
Delivery as indicated, not necessary for
Caesarian section
-
In-utero intervention remains experimental
Delivery:
-
NBM
-
Ryles tube insertion
-
Prompt intubation, avoid bagging as may distend
stomach and worsen condition. Difficulty to ventilate in unknown cases should
have high index of suspicion.
-
Avoid excessive bagging as high risk of
barotrauma and pneumothorax.
-
Adequate ventilation, pulmonary hypertension and
pulmonary hypoplasia is the main complication of CDH and requires aggressive
ventilatory support.
-
Adequate fluid resuscitation as hypotension may
develop due to pulmonary hypertension.
-
Prompt surgical intervention not needed. Stabilization
of patient and delayed surgery is preferred but lacking of controlled studies.
-
Extracorporeal membrane oxygenation (ECMO) in
certain selected cases.
Surgery:
-
Approach: Subcostal or thoracotomy
-
Reduction of herniated organs
-
Primary repair
-
Placement of prosthesis over repaired diaphragm
-
Muscular and fascial flaps may be used to close
repaired diaphragmatic defects.
-
Closure of abdominal incision might need to be
done in two phases as there might not be enough ‘space’ for the returned
abdominal organs. Silo might be necessary while awaiting for abdominal wall to
expand for closure later.
-
ECMO support if necessary during surgery, but
high risk of mortality from bleeding.
-
Chest tube not routine and only if indicated
(pneumothorax)