Neonatal Stridor
Stridor is a harsh, raspy breath sounds heard during
breathing that may indicate an upper airway obstruction. It may occur during
inspiration, expiration or may be biphasic depending on the location of the
obstruction.
Anatomic and Physiologic Considerations
-
Smaller caliber of airway
-
Higher position and longer epiglottis
-
Lower total lung capacity
-
Increased functional residual capacity dependant
on:
o
Increased respiratory rate
o
Active glottic narrowing during expiration
o
Use of expiratory muslces for respiration
Assessment
Babies with stridor should be assessed further for any
evidence of respiratory distress:
-
Cyanosis
-
Chest retraction
-
Tachypnea
-
Grunting
-
Nasal flaring
Some may present with difficulty in feeding, recurrent
choking or cough.
Investigations:
-
Flexible direct laryngoscopy
-
Rigid direct laryngoscopy
Differential Diagnosis
Supraglottic
-
Laryngomalacia (Commonest cause)
 |
| Omega shaped epiglottis |
Glottic
-
Vocal cord paralysis (Second commonest cause)
-
Laryngeal web
Subglottic
-
Subglottic stenosis
-
Subglottic hemangioma
-
Tracheomalacia
-
Trachea stenosis with complete tracheal ring
-
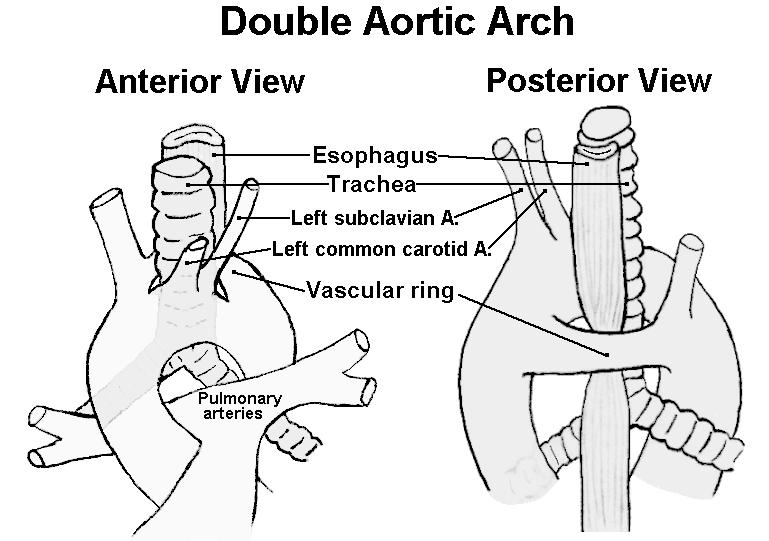
Pulmonary vascular ring
Some websites for demonstrations and information: