Fortunately most term babies are born without complications or needing help for resuscitation. About 10% do and that's a significant number. Basic knowledge of neonatal resuscitation must be available to all medical staffs (doctors and nurses) working in the labour room or the emergency department for that matter as mothers in advanced labour may just pop-up in the emergency department in the middle of the night.
The algorithm above pretty much sums up the steps of neonatal resuscitation covering even babies whom are delivered 'normal' without complications. There are many other variations but this is the one that I'm most used to.
Most times, the outcome of delivery can be roughly predicted even before birth itself.
Knowledge of the patient's history helps a lot in anticipating outcome of delivery.
The initial step as in the box above emphasize the recognition of a baby in need of resuscitation. Four basic questions must be answered:
- Is the baby term?
- Is the liqour clear?
- Is the baby crying or breathing?
- Is the muscle tone good?
If any of the above is
NO, then the next step of resuscitation is required.
Even the first two questions above can be answered before delivery and can be anticipated. With anticipation comes preparation and with good preparation hopefully better outcome may be borne out of the delivery.
If all those answered above are
YES, then the baby maybe passed on to the mother unless otherwise contraindicated, for skin to skin contact and initiation of breast feeding and routine care.
Another interesting note is that
delayed cord-clamping should be practiced (as late as
1 minute after delivery) as there is evidence of reduced incidence of transfusion and increased iron storage in babies with delayed cord-clamping.
INITIAL STEPS TO RESUSCITATION
Below are the basic initial steps for resuscitation. All these steps are to be done ideally within 30 minutes and the baby reevaluated afterwards to assess success of resuscitation and need to proceed with the next step.
Provide warmth and Dry
- Baby is to be placed under radiant warmers.
- If baby is preterm, best to be wrapped in plastic wrappings as preterms are more likely to lose heat more easily
Position and maintain airway
- Positioned in sniffing position.
Stimulate
- Only back stimulation is necessary up to 2 to 3 times.
- Slapping the feet of babies should not be in practice today.
*Clear airway
- Latest guidelines from WHO states that babies whom are breathing on their own should not have regular suctioning, even if meconium was present.
- Suctioning should only be done if there are evidence of excessive secretions.
- There is no evidence in improved outcomes in babies suctioned intrapartum (after delivery of head, before delivery of shoulder) when meconium is present.
- If meconium is present and baby is not *vigorous, direct-suctioning with the meconium aspirator should be initiated straight away, even before positive pressure ventilation is performed.
- Direct suctioning is done until airway produces clear returns or baby becomes bradycardic.
*vigorous = not breathing, limp, heat rate <60 bpm.
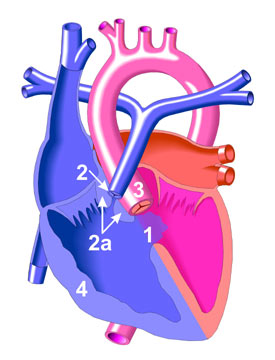
POSITIVE PRESSURE VENTILATION (PPV)
- If the baby is still apneic or heart rate is less than 60 bpm after the initial steps, positive pressure ventilation should be initiated.
- 40 to 60 cycles of breath should be given per minute.
- Ensure there is chest rise. If not, reposition in sniffing position.
- Intubation is to be considered if unable to ventilate.
- Excessive pressure or 'bagging' must be avoided for risk of pneumothorax.
- Heart rate is to be evaluated after 60 seconds of PPV with target > 100 bpm.
- SpO2 monitoring may be attached during the resuscitation, best SpO2 probe to be placed at pre-ductal areas ie. right hand. One must be aware that oxygen saturation is not maximal in the newborn till at least 10 minutes after delivery.
Preductal SpO2 According to Duration after Birth
- 1 minute - 60-65%
- 2 minutes - 65-70%
- 3 minutes - 70-75%
- 4 minutes - 75-80%
- 5 minutes - 80-85%
- 10 minutes - 85-95%
CHEST COMPRESSIONS
- PPV and adequate ventilation should be done before initiation of chest compressions.
- Chest compressions done if heart rate < 60 bpm.
- Best to be done with 2 thumbs on the sternum with the other fingers around the baby for better control of pressure.
- Depth of compression should be 1/3rd of the AP diameter of the baby.
- Ratio of breath to compressions should be 1:3.
- 2 finger technique done if space is needed for procedures ie. insertion of umbilical catheters.
- Intubation must be considered at this stage if not earlier.
MEDICATIONS
- Rarely are medications need in neonatal resuscitation (as compared to adult resuscitation),
- If compressions are ineffective, IV adrenaline 0.01 - 0.03 mg/kg is to be given via intraumbilical venous catheter. If not, adrenaline 0.05 - 0.1 mg/kg may be administered through an endotracheal tube.
- Adrenaline should be diluted in 1:10000 (0.1 mg/mL)
- Adrenaline may be repeated every 3 to 5 minutes if heart rate remains < 60 bpm.
- IV bolus of N/S or HM 10 mL/kg may be given in suspected hypovolemia or anemic babies.
- Naloxone should not be given routinely.
Other Points:
- Remember that resuscitation of the neonate should
NOT be done alone.
- Always call for help of someone more experienced.
- Know what is available ie. laryngeal mask airway may be beneficial
- Know when to quit (Perhaps I'll write about this in other articles)
- And always inform the mother or parents of what was done and why and the outcome.
- Remember documentation.
That's it for now. This is just a 'short-note' of mine that I hope will be beneficial for me and to whoever that reads this. It's definitely incomplete but I hope will cover more of the basic stuff. Future related articles that I'll be posting may be on intubations, UVC insertions, other methods of ventilations, and withdrawing treatment, all important aspects of neonatal resuscitation. Let's hope that I've obtained at least a certificate for NRP by then :D
References:
- Neonatal resuscitation Textbook 5th Edition.
- Special Report - Neonatal Resuscitation, 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, PEDIATRICS, Journal of American Academy of Pediatrics
- WHO Guidelines on Basic Newborn Resuscitation 2012.